Hidden Signs of Depression in Men You Shouldn't Ignore
Share
When we picture depression, we often think of sadness and tears. But for men, it frequently doesn't look like that at all. The classic signs we’re taught to recognise often get missed because they show up disguised as something else entirely – think anger, irritability, or even physical complaints like headaches and stomach problems.
Societal pressure and old-fashioned ideas about masculinity play a huge role here. Men are often pushed to express emotional pain in ways that get brushed off as stress or just a "bad mood," which means they miss out on getting the right support when they need it most. Addressing mental health openly is not just an individual responsibility; it's a societal one that strengthens families, communities, and workplaces.
Why Depression in Men Often Goes Unseen
Depression isn't a one-size-fits-all experience. While we might associate it with persistent sadness, the signs in men can be much harder to spot and are easily dismissed. From a young age, many men are taught to be stoic, to be resilient, and to always be in control, which makes showing vulnerability feel almost impossible.
This pressure cooker environment means that admitting to feelings of hopelessness or worthlessness can feel like admitting failure. Because of this, a lot of men either don't realise their symptoms are actually depression, or they actively hide their struggles behind a mask of strength. This leads to a dangerous silence where the pain is left to bubble away under the surface.
This isn't just a feeling; the numbers back it up.
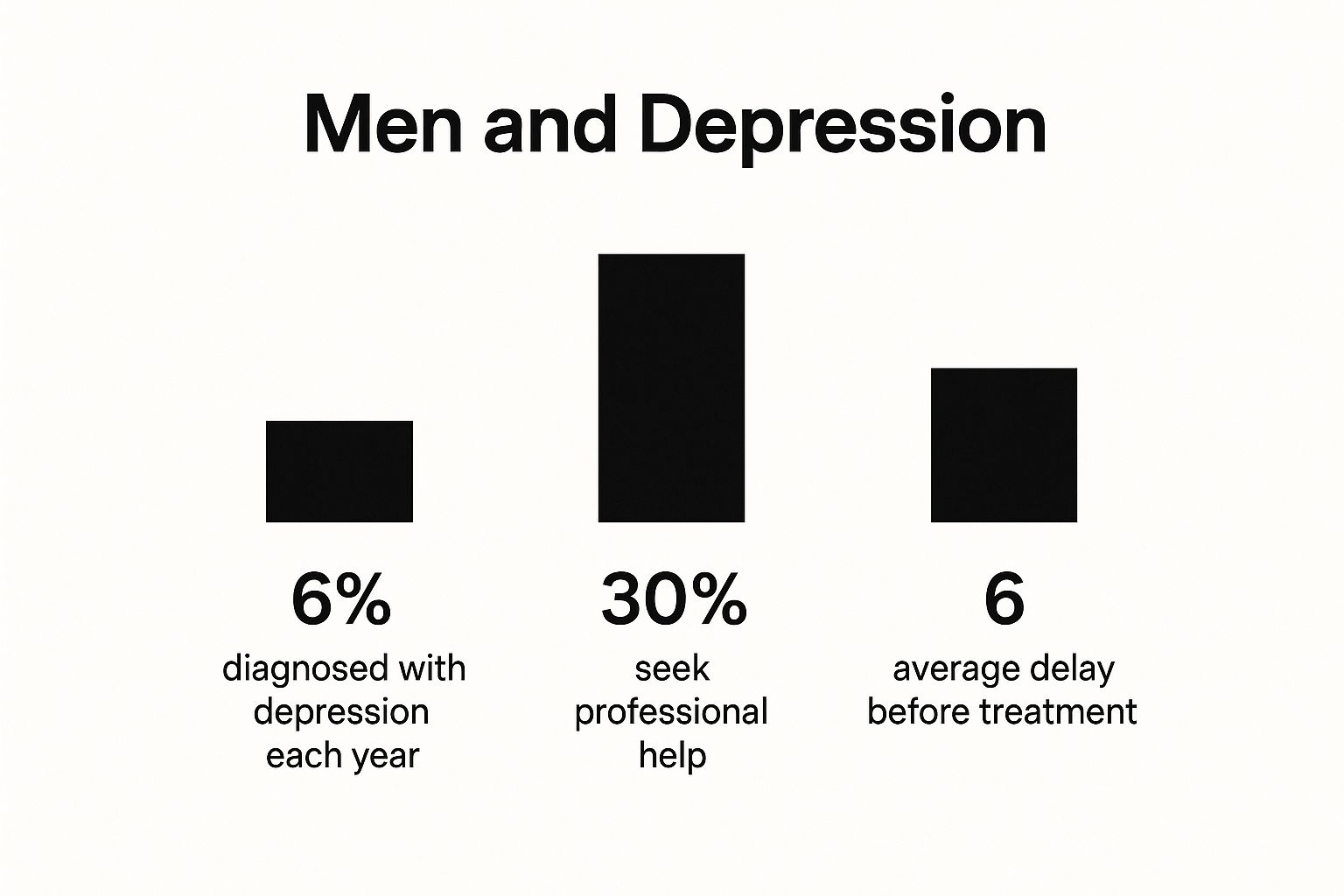
This data paints a clear picture of the disconnect. Far too many men wait months, or even longer, before speaking to a professional, giving the symptoms plenty of time to get worse.
The Misleading Ways Depression Can Show Up
It's helpful to compare what we traditionally think of as depression with how it might actually appear in men. The difference can be stark.
| Classic Symptom | How It May Present in Men |
|---|---|
| Persistent sadness, crying | Irritability, a short temper, or sudden angry outbursts. |
| Loss of interest in hobbies | Working excessively long hours or withdrawing from family. |
| Feelings of worthlessness | Self-criticism and a belief they are failing at work or home. |
| Withdrawing from social life | Spending more time at the pub or using alcohol to cope. |
| Changes in sleep patterns | Staying up late to avoid being alone with their thoughts. |
| Fatigue and low energy | Physical complaints like persistent headaches or stomach issues. |
Seeing it laid out like this makes it clear why it's so easy to miss. Instead of talking about feeling sad, a man might display his distress through his actions. For example, a man who once enjoyed socialising might start cancelling plans, claiming he's too busy with work when, in reality, the effort of pretending to be okay feels overwhelming. That could be a much shorter temper, picking fights over small things, or turning to behaviours that help him escape.
Some common examples include:
- Throwing himself into work to avoid being at home.
- Spending more and more time at the pub or drinking more than usual.
- Taking risks, like driving recklessly or gambling.
These actions often become coping mechanisms—a way to numb the emotional pain or just create a distraction. And because some of them, like working hard or taking risks, can align with traditional ideas of masculinity, they're almost never seen as a cry for help. A big part of the solution is breaking down these stereotypes, something you can read more about in our article on how to reduce mental health stigma.
It's so important to remember that asking for help isn't a sign of weakness. It’s a courageous step toward looking after your health, just like you would for any physical illness.
Ultimately, understanding this context is the first step toward really seeing what's going on. It helps us look past the surface-level behaviour and recognise the potential struggle underneath.
Disclaimer: I am not a mental health professional. The information in this article is for educational purposes only. If you are worried about your mental health or that of someone you know, please consult a doctor or a qualified healthcare provider for diagnosis and advice.
Decoding Emotional and Behavioural Changes
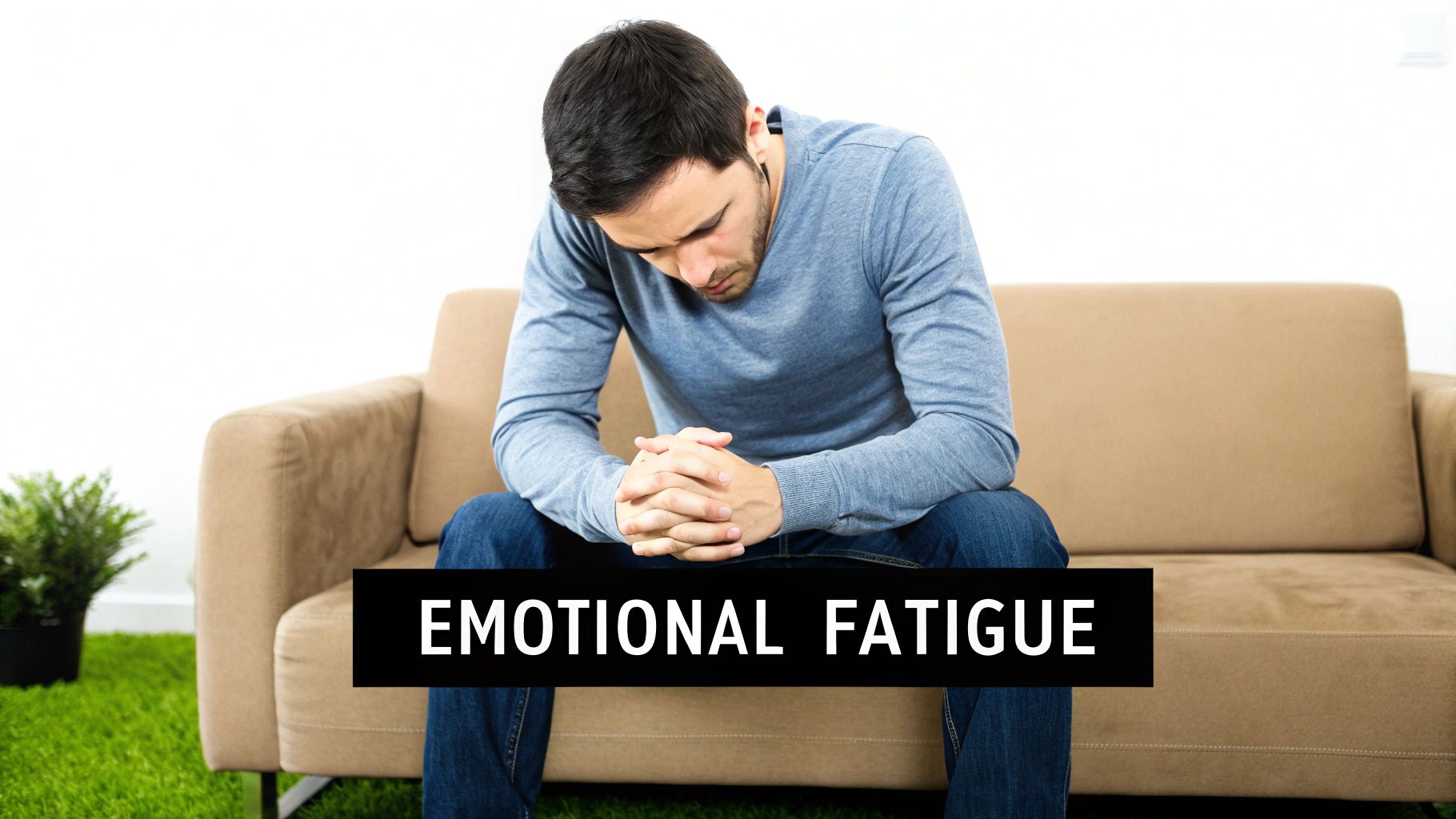
When depression takes hold in a man, it often doesn't look like the profound sadness we see in films. The emotional shifts can be far more subtle, or even look like something else entirely. You might just notice a much shorter fuse.
A minor inconvenience, like being cut off in traffic, can trigger an uncharacteristic burst of road rage. At home, it might show up as snapping at loved ones over trivial things—the TV being too loud or a misplaced set of keys. This heightened irritability isn't some newfound personality flaw; it's often a key sign of a deeper emotional struggle, a way for internal pain to find an external voice.
Alongside this anger, you might see an increase in what we call 'escapist' behaviours. These are things we do to numb or sidestep difficult feelings, and they can easily be mistaken for simple hobbies or a strong work ethic. A crucial first step is to develop self-awareness, as this is the tool that lets us spot these subtle signs for what they really are.
The Rise of Escapism and Withdrawal
Escapism can take many forms, often hiding in plain sight. It’s not just about retreating from the world, but about burying yourself in distractions to avoid being alone with your thoughts.
Here are a few practical examples of what this can look like:
- Workaholism: A man might start working excessively long hours. For instance, he might volunteer for every extra project, not because he's chasing a promotion, but because the office provides a structured distraction from the quiet turmoil at home.
- Digital Retreat: He could spend hours lost in video games or scrolling endlessly on his phone, creating a digital wall between himself and his real-life responsibilities or relationships.
- Increased Alcohol Use: That single pint after work might quietly turn into several, used not for socialising but as a switch to turn off his mind.
This pattern of avoidance also bleeds into social connections. For a man with depression, social withdrawal doesn't always mean becoming a total recluse. He might still show up to gatherings but remain noticeably disengaged, contributing little and leaving early. He’s physically there, but emotionally absent, having lost the energy to connect in a meaningful way. Building stronger inner fortitude is key to managing these impulses, and our guide on how to build emotional resilience offers some practical strategies.
The constant pressure to appear "fine" can be exhausting. Escapist behaviours offer a temporary release from this pressure, but they often deepen the sense of isolation in the long run.
The Impact of the Digital World
In our hyper-connected world, social media adds another layer of complexity. The curated perfection we see online often fuels a relentless cycle of comparison, making a man feel that his own life, career, or relationships just don't measure up.
This constant stream of others' apparent successes can intensify feelings of worthlessness. Rather than being a source of connection, platforms like Instagram or Facebook can become a stark, silent reminder of what he feels he is lacking, quietly eroding his self-esteem and feeding the depressive cycle. Recognising these behavioural shifts as potential signs of depression, rather than just bad habits, is the first step toward offering genuine support.
Recognising Unexpected Physical Symptoms

We often think of depression as something that happens purely in the mind, an emotional struggle. But its reach extends deep into the body, and for many men, the first clues that something is wrong aren't emotional at all. They’re physical.
This is one of the most overlooked aspects of depression in men. Aches, pains, and a general feeling of being unwell can easily be brushed off as stress, a bad night's sleep, or just getting older.
But when these physical issues become chronic and don't seem to get better with the usual remedies, they might be the body’s way of flagging a deeper mental health issue. Men are often more likely to see a doctor for a physical complaint than an emotional one, making these symptoms a critical, if unexpected, entry point for recognising there’s a problem.
The Body Keeps the Score
One of the most common physical signs is a profound, persistent fatigue. This isn't just feeling a bit tired; it's a bone-deep exhaustion that a full night's sleep doesn't seem to touch. Think of a man who constantly complains of being 'knackered' despite getting eight hours a night. He feels sluggish, his energy has vanished, and even simple tasks can feel like climbing a mountain.
This overwhelming tiredness is often joined by other unexplained physical symptoms.
- Chronic Pain: Nagging backaches, persistent headaches, or muscle soreness that have no clear physical cause can all be linked to depression.
- Digestive Issues: Problems like stomach cramps, constipation, or other changes in bowel habits are common. A man might see his GP repeatedly for digestive trouble, never thinking it could be connected to his mental state.
- Appetite and Weight Changes: You might notice a significant shift. Some men lose their appetite completely and lose weight, while others turn to food for comfort and start gaining it.
It's crucial to understand that these physical pains are not "all in his head." Depression can cause real changes in how the body processes pain signals, making these symptoms genuinely debilitating.
Finding Relief and Seeking Help
When facing these physical symptoms, a few gentle relaxation techniques can offer some initial relief. Simple practices like a daily walk in nature, gentle stretching, or trying a guided mindfulness meditation can help calm the nervous system and ease some of that physical tension. Trying a deep breathing exercise, for example—inhaling for four counts, holding for seven, and exhaling for eight—can be a surprisingly effective way to lower stress in the moment. These are excellent first steps for managing the immediate discomfort.
However, it’s vital to remember that these are coping strategies, not cures. While relaxation tips can certainly help, they are no substitute for a proper diagnosis from a medical professional. If these physical signs persist, it is essential to speak with a doctor.
Please remember, I am not a mental health professional, and this advice is for informational purposes only. If you are worried, booking an appointment with your GP is the most important step you can take. They can help rule out other physical causes and guide you towards the right support for both your mental and physical health.
The Ripple Effect of Untreated Depression
When depression is left unaddressed, it’s never just one person’s problem. Think of it like a stone dropped into a still pond – the ripples spread outwards, touching family, friends, workplaces, and the wider community in ways we don't always see at first. It's so much more than an internal battle; it becomes a shared challenge with far-reaching consequences.
The strain on personal relationships, for instance, can be enormous. Partners often find themselves walking on eggshells, trying to navigate unpredictable moods, irritability, or an emotional void where connection used to be. That once-solid bond can start to feel fragile, leading to painful misunderstandings and a sense of isolation for everyone involved.
This is especially true within families. A parent's mental wellbeing is one of the cornerstones of a child’s emotional development. With 1 in 10 children aged 5-16 now having a diagnosable mental health condition, it is clear that adult struggles can cast a long shadow over the home, subtly shaping the environment and, in turn, a child's own mental health.
The Impact Beyond the Home
These ripples don't stop at the front door; they extend right into the professional world. The cost of poor mental health to UK businesses is staggering, estimated by Deloitte to be as high as £56 billion every single year. This isn't just about people calling in sick; it's about the quiet, hidden drain on productivity and team spirit.
Untreated depression in men is a major contributor to this figure, showing up in a few key ways:
- Absenteeism: Having to take time off work because the symptoms feel too overwhelming to manage.
- Reduced Productivity: Finding it hard to focus, hit deadlines, or simply perform tasks that once felt straightforward.
- Presenteeism: This is the big one. It’s the phenomenon of being physically at work but mentally and emotionally absent. An example could be an employee staring blankly at a screen for hours, achieving very little, because their mind is consumed by feelings of worthlessness. This can be even more damaging and costly than someone not showing up at all.
Tackling the signs of depression in men isn't just about individual wellbeing – it's an economic and societal necessity. When we support men's mental health, we're building stronger families, more resilient communities, and healthier, more productive workplaces for everyone.
Ignoring mental health doesn't make the problem vanish. It just transfers the cost onto relationships, businesses, and society. Proactive support isn't an expense; it's an investment in our collective wellbeing.
The Ultimate Cost of Silence
Ultimately, the silence that so often surrounds men’s mental health carries the heaviest price of all. Here in the UK, men are more likely to express their depression through anger or risk-taking, and around 40% avoid talking about their mental health with anyone.
Tragically, this silence can have fatal consequences. Men account for about four in five suicides, and it's the leading cause of death for men under 35. You can read more on these crucial depression statistics from the Priory Group. These aren't just numbers; they're a stark reminder of why proactive support isn't just helpful—it is, quite literally, life-saving.
How to Start a Conversation That Matters

Spotting the signs of depression in a man you care about is one thing, but taking that next step is what can truly change a life. It's often the hardest part, whether you're worried about a mate or struggling yourself. The key is to come from a place of compassion, not accusation.
Simple, gentle questions can make all the difference in creating a safe space for someone to open up. Try to steer clear of phrases that sound like you're judging them. Instead, just talk about what you've noticed and how it makes you feel.
Think about starting with something like, "I've noticed you haven't seemed yourself lately, is everything okay?" or "You seem to have a lot on your plate at the moment, just wanted to say I'm here if you fancy a chat." These non-confrontational openers leave the door ajar without forcing anyone to walk through it.
Preparing for a Doctor's Visit
If you're the one struggling and have decided to get help, a bit of prep before your GP appointment can make the whole thing feel less daunting. It's completely normal to feel nervous about it, so having a plan can give you a much-needed sense of control.
It really helps to jot down a few notes before you go.
- List Your Symptoms: Write down everything you've been experiencing – the emotional, behavioural, and physical signs – no matter how small they seem. Make a note of how long you’ve been feeling this way.
- Think About Your Questions: What do you want to find out? You could ask about different types of support, what the next steps look like, or what you can do at home to help yourself.
- Be Honest: Remember, your doctor is there to help you, not to judge. Being open about everything, including coping mechanisms like drinking more than usual, will help them get the clearest picture of what's going on.
Your GP is the gateway to professional support. They can discuss treatment options, refer you to therapy services, and help you create a plan to start feeling better. Taking that step is a powerful act of self-care.
Normalising the Conversation and Finding Support
Talking about mental health is definitely getting easier, but that old stigma can still feel heavy. The good news is there are loads of ways to normalise these chats and get immediate support. Even things like the growing popularity of mental health apparel or reading books on the topic can be subtle but powerful conversation starters.
For instance, wearing a t-shirt with a positive mental health message from a brand like That's Okay can signal to others that you're a safe person to talk to. In the same way, sharing something you've learned from a book about wellbeing, such as Matt Haig's Reasons to Stay Alive, can bring up the subject in a really low-pressure way.
For more direct support, there are several fantastic UK-based organisations ready to help.
- Mind: Offers incredible advice and support for anyone experiencing a mental health problem.
- The Samaritans: Provides a free, confidential listening service 24/7. You can call them anytime on 116 123 if you just need to talk to someone.
- Campaign Against Living Miserably (CALM): A leading movement against suicide, offering a helpline and webchat specifically for men.
Please remember, I am not a mental health professional, and this advice is for informational purposes only. If you are worried, reaching out to your doctor or one of these brilliant charities is the most important step you can take towards getting the support you deserve.
Taking the First Step Toward Getting Help
Just recognising the signs we’ve talked about is a massive first step. It's so important to get your head around the fact that for men, depression often doesn’t look like the textbook definition of sadness. It might show up as back pain, anger, or just working yourself into the ground.
For generations, society has hammered home the idea that men should just "get on with it" and suffer in silence. But reaching out for support isn't a sign of weakness; it's a profound act of strength.
Don't just brush these signs off, whether you see them in yourself or in a mate. It’s worth looking into all the different avenues for support. This includes everything from therapy and medication to newer treatments, like exploring how ketamine can help reclaim life beyond depression.
Building a solid support network around you is also a game-changer. For friends and family who want to help but don't know how, something like mental health first aid training can make all the difference.
Important Disclaimer: I am not a mental health professional. This article is for informational purposes only. A proper diagnosis and treatment plan must come from a doctor or a qualified mental health practitioner. Please seek professional help if you are worried.
A Few Common Questions Answered
Can a Man Be Depressed If He Still Functions Well?
Yes, absolutely. This is often called ‘high-functioning depression’, and it’s something we see all the time. Plenty of men can hold down a job, manage family life, and tick all the right boxes on the surface while internally, they’re in a real battle.
It might look like they have it all together, but the effort it takes is immense. Look for the more subtle shifts – a shorter fuse, relying a bit more heavily on a drink to unwind after work, or gradually dropping hobbies that once brought him joy. That ability to just ‘get on with it’ can be a powerful coping mechanism, but it often masks serious distress. That's why spotting these hidden signs is so crucial.
What’s the Difference Between Stress and Depression?
This is a great question. Think of it like this: stress is usually a reaction to a specific, external pressure. It could be a looming deadline at work or a family argument. Once that situation is resolved, the stressful feelings tend to ease up.
Depression, on the other hand, is a much deeper and more persistent state. It's a low mood, a feeling of hopelessness, or a total loss of interest that hangs around for weeks or even months, often without one single, obvious trigger. While constant stress can definitely pave the way for depression, the key difference is that depression colours everything. It doesn’t just disappear when a tough project at work is finished; it affects relationships, physical health, and how you see the world.
How Can I Support My Partner Without Pressuring Him?
Navigating this requires a gentle touch. The most effective support comes from a place of non-judgement and genuine care. Start by expressing your concern from your own perspective, using ‘I’ statements like, ‘I’ve been worried about you lately because you seem so tired’. This feels less like an accusation and more like an invitation.
Offer to listen without jumping in to ‘fix’ things. Sometimes, just having the space to talk without fear of being judged is the most powerful thing you can offer.
A simple act of compassion can create a safe space where he feels he can open up without fear of being judged.
You could also try taking small, practical tasks off his plate to lighten his load, or suggest low-pressure activities you can do together, like just going for a walk. Sometimes, even bringing up the topic through cultural touchpoints like mental health books or our own apparel can normalise the conversation, making it feel less intense and more approachable.
Remember, this article is here to provide information, but I am not a mental health professional. If you are truly worried, the most important step you can take is to gently encourage him to have a chat with his doctor.
At Little Fish Books, we believe in nurturing emotional wellbeing right from the start and supporting mental health conversations for everyone, no matter their age. Take a look at our collection of children’s emotional literacy books and our supportive mental health apparel for adults. Visit us at https://thatsokay.co.uk to find resources that can help get these vital conversations started.
