What Is Trauma Informed Care Explained
Share
When we talk about trauma-informed care, we're not talking about a specific type of therapy or a clinical technique. Instead, it’s a profound shift in perspective. It’s about learning to ask, “What has happened to you?” rather than “What’s wrong with you?”. I am not a mental health professional, and this guide is for informational purposes only. If you are worried about your own or a child's mental health, it is essential to seek help from a GP or a qualified professional.
This approach starts with the understanding that difficult, adverse experiences are more common than we might think, and they can leave a lasting mark on a person’s health and behaviour. The goal is to create environments where people feel genuinely safe, understood, and supported.
Understanding the Shift to Trauma-Informed Care

At its heart, understanding what is trauma-informed care means seeing the deep, often invisible line connecting past adversity to present wellbeing. It’s a framework built on compassion, one that completely reshapes how services are delivered across settings like schools, healthcare, and community centres all over the UK. This entire approach is built on the simple awareness that tough life events are common, with studies showing a huge portion of adults have lived through at least one traumatic event.
This model is especially vital when it comes to children's mental health. We now know that adverse childhood experiences can literally change a child’s developing brain, impacting everything from their ability to manage emotions to how they behave in a classroom. In the UK, one in six children aged 7 to 16 has a probable mental health problem. A trauma-informed lens helps us see that what might be labelled as 'disruptive' behaviour is often just a child's way of coping with overwhelming feelings they don't have the tools to handle yet.
A New Way of Thinking
This isn't just a small tweak; it's a philosophical overhaul. It’s about moving away from systems that can accidentally cause more distress and towards ones that actively promote healing and resilience. To do this, everyone involved—from teachers to doctors—needs to understand the signs of trauma and adjust how they interact to build trust and, crucially, avoid re-traumatising someone.
To really grasp this change, it helps to see the old and new ways of thinking side-by-side.
The Shift from a Traditional to a Trauma-Informed Viewpoint
| Traditional Viewpoint | Trauma-Informed Viewpoint |
|---|---|
| Focuses on the person's 'problem' or diagnosis. | Seeks to understand the whole person and their life experiences. |
| Asks, "What's wrong with you?" | Asks, "What happened to you?" |
| Views behaviour as a symptom to be managed or fixed. | Sees behaviour as a form of communication or coping strategy. |
| Can lead to feelings of blame and stigma for the individual. | Reduces stigma by acknowledging the impact of external events. |
| The system is rigid; the person must adapt to it. | The system is flexible and adapts to support the person's needs. |
| Prioritises compliance and control. | Prioritises safety, trust, collaboration, and empowerment. |
Seeing it laid out like this makes the difference crystal clear. It’s a move from judgement to compassion, from fixing a problem to supporting a person.
This mindset has been powerfully brought into the mainstream conversation. A key book shaping this new understanding comes from Oprah Winfrey and Dr. Bruce D. Perry; you can explore the insights from 'What Happened to You?' to see how it champions this compassionate shift. It's a philosophy that puts power back in the hands of individuals by giving them a voice and choice in their own journey.
Creating resources that reflect this empathetic approach is so important. For example, reading the story behind a children's mental health book shows just how these principles can be put into practice to support young minds. By building safe, predictable, and caring environments, we help lay the foundations for lifelong emotional wellbeing.
The Reality of Trauma-Informed Care Across the UK

While the ideas behind trauma-informed care are sparking conversations everywhere, putting them into practice across the UK isn’t a single, tidy story. It’s less like a national mandate and more like a patchwork quilt. Different regions are weaving their own unique patterns, driven by local needs, resources, and passionate leaders.
This grassroots energy is incredibly powerful. All over the country, individuals and local authorities are stepping up, creating networks to share what’s working and pushing for change from the ground up. But this approach also shines a light on a major hurdle: creating a consistent standard of care for every child, everywhere.
A Patchwork Approach to Implementation
The journey to becoming truly trauma-informed looks very different depending on where you are in the UK. The conversation is happening nationwide, but the actual level of strategic planning and integration varies wildly.
Right now, trauma-informed care in the UK is defined more by this piecemeal adoption than any unified national strategy. Scotland and Wales have made more coordinated, top-down efforts to embed these principles deep within their public services. England, on the other hand, has seen more of a bottom-up movement. It's often championed by dedicated trauma leads and local councils who form their own networks to drive progress.
Despite its growing recognition in health and social care, the absence of a cohesive nationwide policy gets in the way of consistent application and fair funding. To get a better sense of the current situation, you can explore the findings on trauma-informed approaches in UK healthcare.
This reality creates a complicated picture. On one hand, the local passion is inspiring and results in solutions that are genuinely tailored to the community. On the other, it can lead to a postcode lottery, where the support a child and their family receives depends heavily on the specific initiatives available in their area.
Challenges on the Path Forward
For what is trauma-informed care to become a sustainable, standard practice across Britain, we need to tackle several key challenges. One of the biggest is the need for consistent, high-quality training that’s available to all professionals working with children and families, from teachers to social workers.
Another vital step is building a solid UK-specific evidence base. While the core principles are well-established, we need data on what works best within our unique healthcare, education, and social care systems. This won’t just prove the value of the approach; it will guide future investment and policy.
A shared national vision, backed by proper funding and better coordination between organisations, is essential. Without it, even the most passionate local efforts risk staying isolated, holding back the widespread, systemic change that is so desperately needed.
Ultimately, the goal is to move beyond a collection of inspiring local projects to a fully integrated national standard. This is how we ensure every child, regardless of their postcode or background, can benefit from an environment that truly understands what has happened to them and is ready to help them heal and thrive.
The Six Pillars of a Trauma-Informed Approach
So, what does it actually mean to be ‘trauma-informed’? To get to the heart of it, we need to look at the foundations. Think of it like building a house – without strong pillars holding everything up, the whole structure is unstable. The Substance Abuse and Mental Health Services Administration (SAMHSA) gives us six core principles that act as these essential pillars.
These aren't just buzzwords or abstract ideas. They are practical, real-world commitments that can transform an environment. They shift a setting from one that might accidentally re-traumatise a young person to one that actively and intentionally promotes healing.
Let’s break down each pillar and see what it looks like in practice, say, in a UK school or youth club.
1. Safety
This one is the absolute, non-negotiable starting point. It’s about creating safety in every sense of the word – not just physically, but psychologically, too. A child has to feel secure in their surroundings and safe in their relationships with the adults around them.
- What this looks like: In a classroom, it could be as simple as having a predictable daily routine written clearly on the board. When children know what’s coming next, it reduces anxiety. It also means an adult who uses a calm, steady tone of voice, even when a child is distressed, creating an atmosphere of emotional reliability and security.
2. Trustworthiness and Transparency
Trust is the glue that holds any supportive relationship together. This pillar is all about being reliable, consistent, and completely open in every interaction. Decisions are made with transparency, not behind closed doors, and there are no hidden agendas.
- What this looks like: A youth club leader who clearly explains the rules and, crucially, the reasons behind them is building trust. If a much-anticipated trip has to be cancelled, they explain why honestly instead of being vague. This consistency helps young people to believe what adults say and rely on them. For example, if a promised activity is changed, explaining "The weather forecast is for heavy rain, so we'll do the indoor craft session instead to stay safe and dry" builds much more trust than a vague cancellation.
3. Peer Support
This principle acknowledges the incredible power of shared experiences. There's something deeply validating about connecting with others who have been through similar struggles. It fosters a powerful sense of belonging and shows a young person they aren't alone in what they're feeling.
- What this looks like: A school might set up a ‘buddy system’ where older students mentor younger ones. That friendly face and listening ear from a peer can feel much less intimidating than talking to an adult, making it easier for a child to feel heard and understood.
4. Collaboration and Mutuality
Here’s where we dismantle the old ‘us vs. them’ dynamic. This is about levelling the power imbalances that so often exist between adults and young people. It’s about working with people, not doing things to or for them. Every voice matters, and everyone has a role to play.
- What this looks like: Instead of a teacher simply laying down the law, they might hold a class meeting to create a shared agreement on how everyone wants to be treated. This simple act gives children a sense of ownership and shows them that their input is genuinely valued. A practical example is a family agreeing on house rules together, where children help decide on consequences, fostering a sense of fairness and mutual respect.
5. Empowerment, Voice, and Choice
Traumatic experiences often strip people of their sense of power and control. This principle is all about giving that back. It means truly listening to what individuals have to say and, wherever possible, giving them a real choice in the decisions that affect their lives.
- What this looks like: When a child is upset, a carer might say, “I can see you're feeling really overwhelmed. Would you like to spend five minutes in the quiet corner, or would you prefer to draw at your desk?” This simple choice gives the child agency over their own coping strategy, which is incredibly empowering.
6. Cultural, Historical, and Gender Issues
Finally, this pillar demands that we move beyond any kind of one-size-fits-all approach. It’s about recognising that a person's entire background—their culture, race, gender, sexuality, and personal history—shapes their experience of the world and their trauma. It’s a commitment to actively moving past stereotypes and biases to see the whole, unique person in front of us.
- What this looks like: A support worker makes sure the books, posters, and resources in their space represent diverse families and backgrounds. They also take the time to learn about and respect the cultural norms of the young people they support, ensuring their services feel relevant, respectful, and truly inclusive.
Why This Approach Is Vital for Children's Mental Health

A child’s world is one of constant growth and discovery, and their brain is incredibly sensitive to everything happening around them. This is why understanding what trauma informed care is isn't just a helpful extra—it's completely non-negotiable for anyone supporting young people today.
Experiences, both good and bad, don't just create memories; they physically shape the developing pathways in a child's brain.
Adverse childhood experiences (ACEs) can have a truly profound impact, influencing everything from a child's ability to manage their emotions to how they behave at school. With around three children in every classroom living with a mental health issue, an empathetic, informed approach is absolutely essential. The cost of not addressing these issues is enormous, not just for individuals but for society. In the workplace, mental ill health costs UK businesses approximately £56 billion per year.
Seeing Behaviour Through a New Lens
Think about a young person in class who frequently shouts out, interrupts, or just can't seem to sit still. The traditional view might label this behaviour as ‘disruptive’ or ‘defiant’, usually leading to some sort of punishment. But a trauma-informed lens asks a different, more powerful question: what is this behaviour actually communicating?
Often, what we see as misbehaviour is a child's desperate attempt to cope with overwhelming feelings they can't otherwise express. Their nervous system might be stuck on high alert, and their actions are simply trying to find a sense of safety or control.
Responding with punishment only makes them feel more threatened, locking them into a negative cycle. Instead, responding with compassion and support helps them learn the skills they need to manage those big feelings.
This shift from punishment to support is the cornerstone of fostering true resilience. It teaches a child that even when they feel overwhelmed, there are safe ways to cope and trusted adults who will help them, rather than isolate them.
Understanding the complexities of family life, such as coping with co-parenting challenges, especially with a narcissistic parent, really highlights how crucial a trauma-informed perspective is for protecting a child's wellbeing.
Navigating Modern Pressures
Today’s children are also navigating pressures that were completely unimaginable just a generation ago. Social media, for instance, can create a relentless cycle of comparison, cyberbullying, and anxiety. For a young person, a single negative comment online can feel deeply personal and incredibly distressing, fuelling poor self-esteem and feelings of isolation.
A trauma-informed adult recognises this. They understand that a child who is suddenly withdrawn or acting out might be reacting to something that happened on their phone only moments before.
This perspective allows for a response rooted in empathy, opening the door for a conversation instead of slamming it shut with judgement. Ultimately, it gives adults the tools to help the next generation not just survive, but truly thrive. There are many simple and effective ways you can start making this difference; for more ideas, you can explore these 4 things you can do to support your child's mental health.
Putting Trauma-Informed Principles into Daily Practice
Knowing the theory behind trauma-informed care is one thing, but the real magic happens when we weave those ideas into our everyday interactions. It’s all about making small, deliberate shifts in our homes, schools, and communities to create places where young people feel genuinely safe, heard, and valued.
This isn’t about trying to be a therapist. Far from it. It’s about being a dependable, trusted adult in a child’s life. Think about how predictable daily routines can give a child a sense of stability when their world feels chaotic. Simple things, like consistent mealtimes or a regular bedtime story, build a foundation of safety that can help lower stress and anxiety.
A huge part of fostering this environment of safety and trust comes down to how we talk. Using effective therapeutic communication techniques is key. This could be as simple as gently starting a conversation about feelings, maybe by using emotions colouring sheets or just asking, “I noticed you seemed a bit quiet today. Is there anything you’d like to talk about?”
Building a Supportive Environment
Creating a supportive atmosphere is about more than just good intentions; it requires consistent effort and the right tools to help open up conversations about mental wellbeing. It's about our actions and the resources we use.
Here are a few practical ideas you can try:
- Simple Relaxation Tips: Teach children simple breathing exercises. A brilliant one is ‘box breathing’: breathe in for four seconds, hold for four, breathe out for four, and hold again for four. It’s a simple activity that can be done anywhere to help calm an overwhelmed nervous system. Another is the 5-4-3-2-1 grounding technique: notice 5 things you can see, 4 you can touch, 3 you can hear, 2 you can smell, and 1 you can taste.
- Mental Health Books: Reading stories together about feelings and resilience can be a powerful and non-intrusive way to explore tricky subjects. Well-chosen books like The Worrysaurus by Rachel Bright or Ruby's Worry by Tom Percival can give children the language they need to express what they’re feeling inside.
- Mental Health Apparel: Sometimes, something as simple as a T-shirt or hoodie with a positive message can be a quiet conversation starter. For both adults and young people, wearing apparel that supports mental health awareness helps to normalise the topic and show solidarity.
An Important Disclaimer
I want to be absolutely clear: I am not a mental health professional. The information in this article is for educational purposes and should never be a substitute for professional medical advice. If you are ever worried about your own or a child's mental health, please seek help from a GP or a qualified mental health professional.
For those looking for more guidance on this topic, you might find our guide on effective strategies for providing youth emotional support helpful.
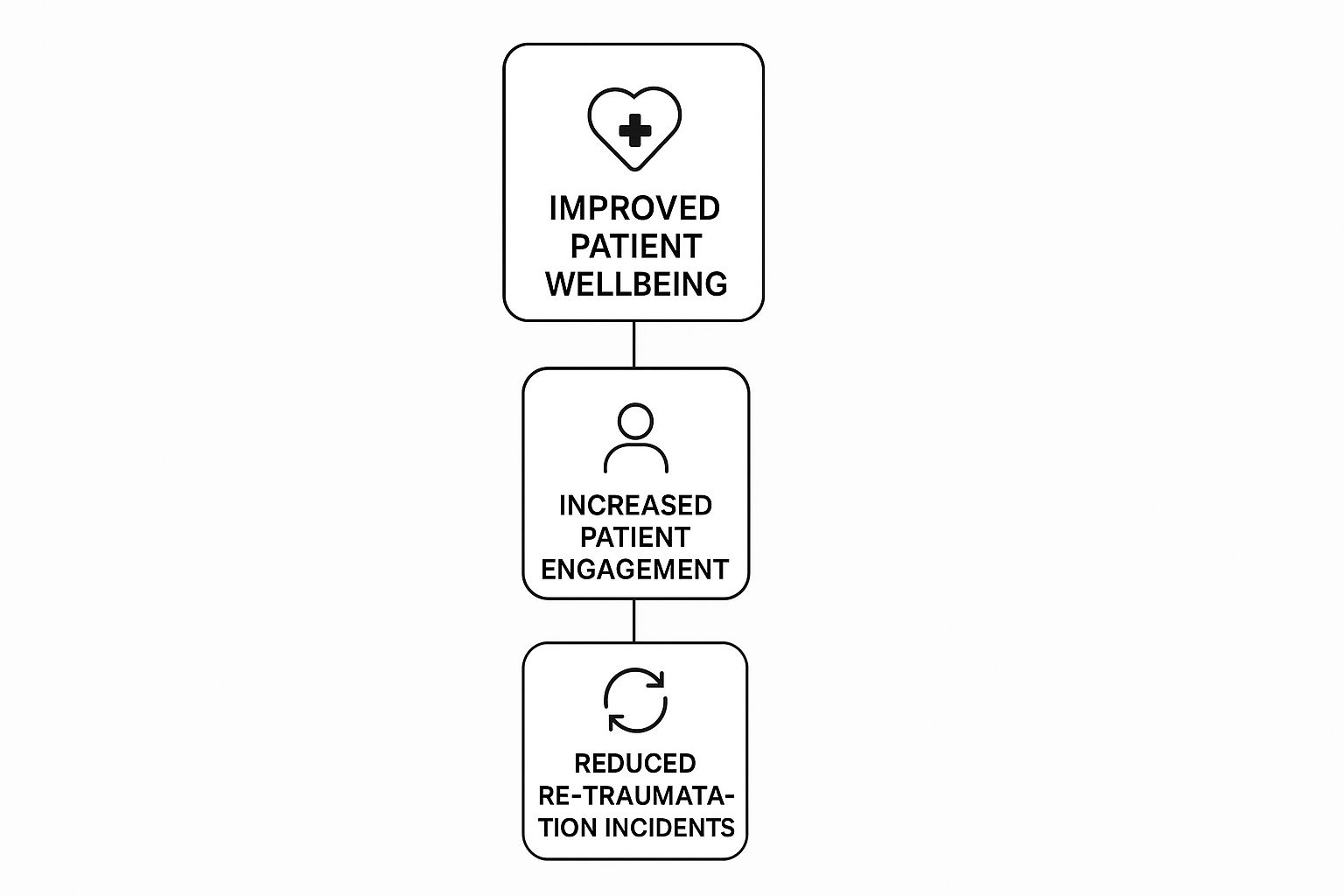
The need for structured, evidence-based approaches is undeniable. Research from the UK has shown that successful trauma-informed programmes depend on strong workforce training, thoughtful policy development, and collaboration. These elements are crucial for reducing the risk of retraumatisation and improving health outcomes for everyone involved.
Still Have Questions? Let's Clear a Few Things Up
How Is This Different From Just Being Kind?
That’s a great question, and it gets to the heart of the matter. While kindness is absolutely essential in any human interaction, trauma-informed care is something more specific and intentional.
Think of it this way: kindness is like offering someone a warm drink on a cold day. It's a lovely, helpful gesture. Trauma-informed care, on the other hand, is like being an architect who designs a building with central heating, insulation, and storm-proof windows from the very beginning. It's a proactive, structural approach.
It's rooted in a real understanding of how difficult experiences can shape a young person's brain and behaviour. It means we actively change our routines, communication, and even our physical spaces to support healing, not just react nicely in the moment.
Is This Only for People with a PTSD Diagnosis?
Not at all. This is a common misconception. Trauma-informed care is a universal approach, a bit like universal design in architecture that makes buildings accessible for everyone, not just those with a visible disability.
It's based on the idea that we can never truly know what someone has been through. By creating an environment that is safe, respectful, and empowering for everyone, we ensure that we're supporting those who have experienced trauma, whether they have a diagnosis or not. It's about promoting dignity and understanding across the board.
Can I Use These Principles at Home as a Parent?
Absolutely! In fact, many parents find these principles transform their relationship with their children. Core ideas like creating safety through predictable routines, building trust, and offering choice (with age-appropriate control, of course!) are fantastic parenting tools.
They help you look beyond a behaviour and understand the why behind it. This shift in perspective allows you to respond with more empathy and connection, which strengthens your bond immeasurably.
Important Note: This article is for informational purposes only. I am not a mental health professional. If you have concerns about a child's mental health, please consult your GP or a qualified professional for guidance.
At Little Fish Books, we create resources designed to gently open up conversations about feelings and resilience. Explore our collection of books, activities, and supportive apparel to help nurture emotional wellbeing in the young people you care about. Visit us today to find tools that build stronger connections.
Article created using Outrank
